Everything You Need to Know: Arthroscopy and Arthrocentesis Surgeries for TMD

If you have TMJ Disorder, you’ll be familiar with the fact that there are no agreed upon treatments or cures. Each physician/specialist has their own biases as to what treatments work best, claiming all the others are bull. However at this point there is at least somewhat of a consensus that surgery should be a last resort.
There’s a lot of validity to this. When it comes to open jaw surgery, whether it be resetting the position of the disc your jaw slides on, or completely replacing parts of the TMJ mechanism, there is a tremendous amount of risk. Flat out, the majority of patients that undergo open jaw surgery will at some point have TMD symptoms return at the same levels if not worse. This is because the jaw joint is one of the most complex in the human body. “Fixing” one part of it will inevitably cause an imbalance in the system and will result in disorder somewhere else. This isn’t even to mention the horrible multi-month recovery process of a body part you use to eat, drink, and talk. This is why only in the worst cases of joint degradation should someone even consider such a procedure.
But over the last decade, 2 surgeries have been gaining traction within Orofacial surgeons - minimally invasive, low risk, and often displaying an 80% success rate in improving quality of life. In this article, we’ll be diving into both the Arthroscopy and Arthrocentesis surgery of the TMJ.
Before diving into the surgery though, it’s important to understand what’s going on inside the joint that causes all the pain, tension, and lockups. I want you to understand that there is such a complex interplay between all the muscles in the area, the joints, ligaments, soft tissues, and lifestyle that there is no simple explanation that covers all cases of TMD. However there’s a good chance regardless of the underlying reason, inflammation ends up being a player.
Inflammation is a term thrown around a lot in life, but most people don’t really understand what it really is. In general, it’s your body’s natural response to injury, infection, or tissue damage. It’s characterized by increased hormone release that mainly results in increased blood flow in the area that brings immune and repair cells and proteins. But those same hormones also trigger pain response from the surrounding nerves. For short periods, inflammation is a good thing. But in many cases, inflammation in the jaw joint becomes chronic. For example, this can come from traumatic injury, long term stress/overuse, or even muscular imbalances that cause disc displacement.
Disc Displacement: The articular disc is the piece of tissue that cups your “condyle” (the end of your jaw joint). Normally, this disc slides back and forth as you open and close your jaw. However sometimes due to many possible reasons, this disc can be pulled out of place. This is the reason for clicking for example, where your jaw pops in and out of the disc as you open and close. But a misaligned disc can also result in pressure on soft nervous tissue in the TMJ, a common cause for pain. If the disc displacement continues to get worse, it can get folded or stuck in front of the jaw joint, resulting in a “closed lock” as well. While it’s important to note that neither the Arthroscopy nor Arthrocentesis returns your TMJ to its correct anatomical state, bad disc displacement can be a cause for chronic inflammation, which is the main focus of the surgeries.
What chronic inflammation does to the joint:
Basically the immune cells and proteins that play a part in repair and healing of damaged tissue aren’t perfect. There is always some damage to healthy tissue that occurs in this process. In the short term, this damage is marginal. However in cases of chronic inflammation, a vicious loop is created. After long enough, the damage to healthy tissue builds up, increasing inflammation, and in result increasing damage done. This is exactly what arthritis is. Over time scar tissue builds as well and starts to limit the movement of the joint until one day it can completely fuse.
Even in early stages, inflammation can result in fibrous scar tissue called adhesions that form between different tissues in the TMJ. At first, these adhesions are super thin and flexible, and don’t impact range of motion. But as time goes on you can develop more and more adhesions that can thicken, grow veins, and stiffen. This can not only cause more pain, but also restricts your body from adapting to displacements in the jaw (makes mechanical blockage form the disc permanent).
So now we’re ready to understand what the goal of the Arthroscopy and Arthrocentesis surgeries are.
Arthroscopy is a surgery that mainly uses an arthroscope. This is basically a small tube that contains a camera and sometimes small surgical tools. Surgeons make a small incision in front of the ear like the one below to insert this device.

This allows the surgeon to see exactly what’s going on in the joint, with the main goal of locating adhesions and areas of high inflammation. Often these adhesions can be ruptured using the arthroscope, which can instantly help with range of motion if the adhesions were developed enough. Removing early stage adhesions also has the benefit of preventing them from growing and worsening the condition over time.
Here is a picture of an early stage adhesion in the TMJ.

The arthroscopy is also often combined with Arthrosentesis. Arthrocentesis is simply the washing out of the joint. This can be done with synovial fluid (which is the fluid that exists in a joint) or steroids which help mitigate inflammation. The main benefit is to break the cycle of inflammation by washing out some of the looser damaged tissue and swelling. Arthrosentesis is also often done separate from an arthroscopy, however it’s important to note that without seeing what’s going on, it can be less effective. Additionally there is no evidence that you can flush out any adhesions or more attached scar tissue using this technique.
Why are these procedures such a breakthrough in TMD treatment?
Unlike prior techniques, these surgeries aren’t meant to be a last resort. They’re super quick (around 15min per joint), require minimal recovery (you’ll be back to eating normally after a week), and are often effective in preventing further joint damage, improving range of motion, and reducing pain - all with considerably less risk.
Of course as with any surgery there are risks of complications listed below:
- vascular injury;
- extravasation;
- scuffing of cartilage;
- broken instruments;
- otologic complications;
- intracranial damage;
- infection;
- nerve injury.
The surgery is still not meant to be for people with minimal TMD symptoms, and should be reserved when less risky methods have been exhausted, such as Physical Therapy, anti-inflammatories & muscle relaxers, temporary splints, and simple postural changes for example. But once recommended by your physician, the Arthroscopy along with Arthrosentesis can be powerful diagnostic and treatment tools worth considering.
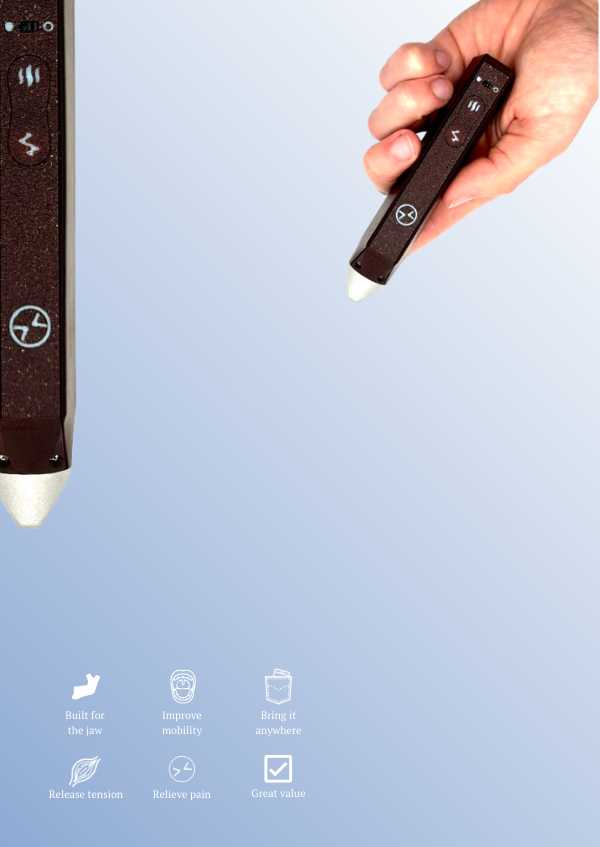
If you found this article interesting or informative, consider following us on instagram @mytmjrelief
Technical Sources:
Arthrocentesis: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6585213/
Intra Articular Adhesions: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2702314/
https://onlinelibrary.wiley.com/doi/pdf/10.1111/j.1834-7819.2002.tb00322.x
Arthroscopy Procedure: https://pocketdentistry.com/33-temporomandibular-joint-surgery-including-arthroscopy/